Carrier Feeds: Getting Started
A summary on carrier feeds, how to set up your carrier feeds, dos and don'ts, and FAQs
Need some extra help with your carrier feeds? Namely offers a wide range of additional services that allow our clients to focus on what matters most—building a better workplace. Check out our Project Services Catalog and see how we can tackle the complex tasks for you.
OVERVIEW
A "Carrier Feed" is another term for an "EligibilityFileFeed", or ElectronicDataInterchange (EDI) file that is sent by Namely to your Carrier. A Carrier Feed may include enrollment, demographic, and/or payroll data depending on the benefit offered. Every Carrier requests their own unique file format and every plan configuration is unique to each client. Namely must go through the following four phases to complete a Carrier Feed Project.
Refer to this video: https://vimeo.com/425904141/a1febf0a49
What is their purpose?
Carrier feeds allow information to be seamlessly sent to an insurance carrier when your employees make changes in Namely. For example, when an employee makes a benefits election in Namely, that change will be sent directly to the carrier via the feed.
In addition, we can set up feeds to financial institutions and to FSA/Commuter/Transit benefit administrators to send payroll contribution information (to communicate 401(k) contributions or HSA contributions, for example).
Note: Carrier feeds send election and account balance information only. They do not send money (i.e. HSA or 401(k) payroll deductions), so while the administrator will get the account balance information it needs via carrier feed, you will still need to set up a separate funds transfer to deposit money into your employees’ accounts.
SETTING UP YOUR CARRIER FEEDS
Timeline
Once Namely begins development on your feed, it can take up to 12 weeks to complete. This timeline accounts for feed construction and testing; however, it can vary and may be shorter or longer depending on data accuracy (ie: a match between Namely and carrier records), carrier responsiveness, testing results, or any difficulty in contacting you during testing.
Enrollment Transfer (pre-feed)
After your benefits administration site is complete, but before the feed is live, there will be a period in which you will need to make sure enrollments are sent to your carriers either manually or through a report. Namely can create these reports on your behalf and show you how to pull them. You or your benefits broker will then need to send the data to the carrier.
To get started, please reach out to your carrier or benefits broker to determine the required format for the manual or custom report. Your carrier may have a web portal or flat file (ie: a census file) for submission. If Namely is acting as your broker, then we’ll help you get this information and manage enrollment transfer pre-feed.
The timing to build a custom report is based on carrier and format. The custom report's needs will be reviewed when requested, and anything outside the scope of your contract may be subject to additional fees.
The Importance Of Testing
We want to ensure that our clients feel comfortable when we go live with a carrier feed. That’s why it’s so critical for us to test and identify errors before launching a new feed—a joint effort that requires you, the carrier, and Namely.
The testing process involves sending a Namely system snapshot to the carrier and comparing that snapshot to the enrollment the carrier has on record. During testing, if the data between Namely and the carrier is not matching up, carriers must be responsive in informing Namely of what the errors are, and then we will inform you and ask you to help us by making changes to the data based on the errors. Please note that we may need your support to resolve data discrepancies in the Namely benefit administration and/or carrier enrollment system as part of the testing process.
Of course, we do not want to turn on a feed that has errors, which could result in unintended enrollment changes for your employees, so we err on the side of caution. When testing has been successful (a.k.a. the information in Namely matches all of the information the carrier has on their end) we will reach out for your final approval to turn the feed on.
Going Live
Once a carrier feed is live, Namely must be your system of record. The carrier feed will send once per week and will ensure that the carrier’s system is updated with any changes confirmed on Namely. As a best practice, all updates should be made in Namely and not directly into any of the carrier portals. The feed will act as your trusted enrollment transfer method, so if enrollment is changed in a carrier portal directly, it is imperative that it also be changed at the same time in Namely.
Possible Speed Bumps
There are a few things that can cause delays in the setup process, specifically:
-
Benefit contracts & associated account structure must be implemented by the carrier before the feed can be set up. The timing of this implementation varies by carrier.
-
During the end of Q4 and through early Q1, many carriers institute black-out periods for all benefits, since it’s their peak season. During this time, these carriers may not accept or work on carrier feeds. Please see Enrollment Transfer (Pre-Feed) above for details about creating a custom report in lieu of a feed.
-
Any changes to the benefit plans (i.e. adding an additional plan with the same carrier) or account structure (e.g. new EIN, Division, Class) must be communicated to Namely and will require the feed structure to be rebuilt and retested. If you are making any of these changes at any time during your relationship with Namely, please let our Service team know (via a Help Community case) that plans are changing, and please ask your carrier to send Namely the updated file specifications to ensure that everything runs smoothly.
CARRIER FEED DO'S AND DON'TS
Do
Before Namely is live (i.e. implementation):
-
Track any enrollment changes, so that you can input them into Namely, once up and running.
-
Provide us, as part of Namely implementation, with the employee and dependent election information (including social security numbers) as soon as possible. Sometimes this information can be time-consuming to gather, but it really speeds up the process when we have it ready to go during implementation.
Before carrier feed is live (i.e. feed development and testing period):
-
Make enrollment updates in both Namely and the Carrier’s system.
After your feed is live:
-
Only make updates to Namely.
-
Properly terminate employees & their benefits in Namely when employees leave your organization so the feed updates accurately. If this is not done, the employee will continue to be active with the carrier.
-
Ensure that you are using the Namely Benefits Administration System regularly for all changes (new hires, terminations, and qualifying life event changes) so that feeds work properly.
Don't
-
Make updates with the carrier, until you have made updates in Namely. Namely should always be the system of record.
-
Enter deductions in Namely Payroll without a corresponding plan enrollment in Namely Benefits Administration. The carrier feed will not transmit if this occurs.
FREQUENTLY ASKED QUESTIONS
Who is responsible for each part of the setup?
-
Namely: We build the feed, make technical adjustments, and provide guidance as to what data needs to be updated in Namely during testing.
-
Client: You maintain accurate data in Namely, and make necessary changes and updates before the week.
-
Carrier: The carrier provides specifications, tests feeds, notifies us of discrepancies and adjustments to the file, sends production reports, and notifies us of any updates or changes in structure.
Is it possible to purchase additional feeds outside of those included in the contract?
Yes, it is possible to purchase additional feeds. Once we have your specifications, we can provide an estimate based on level of effort (measured in hours).
Are there specific carriers you can’t do feeds for?
We will build a feed with any vendor who is willing to build a feed with us. Many carriers have eligibility requirements for file feed connectivity that may factor in size of client, geography, or carrier platform, which can limit our ability to build certain types of feeds. Some carriers will not build a feed for a small group. Even if we can’t build a feed with your carrier, there are several alternate ways to get your enrollments from Namely to a carrier and we are happy to discuss them with you. Feel free to reach out to your contact for benefits for more information.
What number of employees qualifies as a "small group"?
The definition of small group varies by carrier and by state, as does the carrier feed size requirement. Only your benefits broker or carrier can confirm this with certainty.
What information is used for each type of feed (i.e. benefits or deductions)?
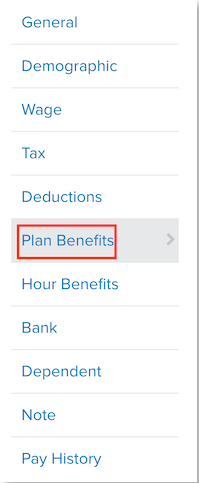
Plans like medical, dental, and vision work off of the Plan Benefits section of Namely Benefits Administration.
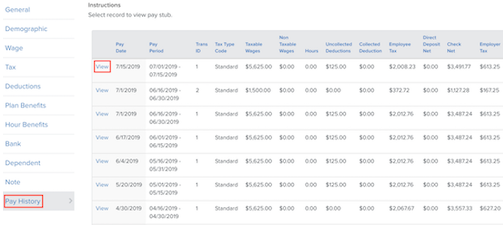
Plans that have funding—such as HSA, FSA, and 401k—pull enrollments from Plan Benefits and their associated payroll deduction which can be seen on an employee’s pay stub.
When are the feeds sent?
Feeds are sent at different times depending on the carrier, but most feeds are sent on Tuesday evenings. If you have questions about a specific carrier, feel free to reach out to our Service team via the Help Community.
Can clients request a different send date?
Namely generally sends feed information on Tuesdays. Exceptions are only made when carriers require a certain day, which happens in rare circumstances.
Will I get a confirmation email from the carrier? What does the confirmation email mean?
Confirmation emails are sent on a per-carrier basis. If you receive emails from your carrier, they will contain data discrepancies that the carrier needs further clarification on or that their system cannot make sense of (e.g. a benefit enrollment beginning prior to a hire date, an employee being terminated over 60 days ago, etc.). You should review this every week, as changes may not be processed without review.