ACA and Transmittal Details for 2022 Reporting
Dear Client,
IMPORTANT:
The ACA Transmittal that has been popping up during payroll will no longer appear after November 4th. If you are required to report, please let CertiPay know immediately so this can be populated on your behalf. Following November 4th, CertiPay will implement a late sign-up fee for 2022 ACA reporting.
PLEASE NOTE: Your ACA filing status can change year to year based on your full time/full time equivalent employee count. If you are unsure if your company is required to report for ACA in 2022, please review the article below.
We are reaching out to inform you that the 2022 ACA Transmittal will be turned on during payroll beginning on September 1st, 2022. Upon processing payroll, you will receive a notification asking if you would like Certipay to file your 2022 1094 & 1095-C forms. You must indicate ‘Yes’ or ‘No’. If you bypass the pop up, it will continue to be displayed each time you process payroll up through the date of November 4th. Once you have indicated ‘Yes’ or ‘No’, the transmittal will no longer appear during payroll. If you indicate ‘No’ that you would not like Certipay to file your 1094 & 1095-C forms, and you are required to ACA report, you will be responsible to do so on your behalf. If you indicate ‘Yes’ that you would like Certipay to file your ACA forms, it is important that you maintain Certipay to ensure your company is in compliance with the Affordable Care Act.
If you said ‘No’ by mistake, or need to make any changes, please reach out to Client Solutions so they can update the transmittal on your behalf.
State Health Mandate Reporting
If your company is required to report for ACA, pay close attention to the ACA state mandate reporting tab on the transmittal. Currently, California, New Jersey, Rhode Island, and the District of Columbia have Individual Mandates in place and require employers to report their ACA information on a state level. Please refer to the state specific links indicated below that will help you determine if you need to report to a specific state.
Certipay offers a standard payroll report named ‘ACA Form 1095-C by State’ that can be found under the ‘Affordable Care Act’ Report Sub Type section under the Reporting tab. You can pull this report by the state you are required to report in to verify which employees will be included in the state reporting for 2022.
California: https://www.ftb.ca.gov/file/business/report-mec-info/index.asp
District of Columbia: https://otr.cfo.dc.gov/sites/default/files/dc/sites/otr/publication/attachments/FAQ%20reporting%20SRP%20Update.3.31.20.pdf
New Jersey: https://nj.gov/treasury/njhealthinsurancemandate/employers.shtml
Rhode Island: http://www.tax.ri.gov/healthcoveragemandate/index.php
ACA Form Filing Fees:
$175 per transmittal Form 1094-C (per EIN) $4.95 per employee Form 1095-C
State Filing Fees:
$175 per state filing $7.50 per applicable employee
How to determine if your company needs to report for ACA in 2022
ACA reporting is required for ‘Applicable Large Employers’ also known as ALEs that have 50 or more full time/ fulltime equivalent employees. The purpose of the annual ACA reporting requirement is to certify that employers are offering minimum essential coverage (MEC) to at least 95% of eligible employees. To determine if your company needs to report for ACA in 2022, you would have had to have 50 or more full time/fulltime equivalent employees that worked for your company in the prior calendar year.
There is a report that you can pull in Certipay called ‘Fulltime/Fulltime Equivalent Employees’ that calculates hours worked for all employees during each month of the calendar year. This report will tell you if you had 50 or more fulltime employees in the previous year.
To locate the ‘Fulltime/Fulltime Equivalent Employees’ report in Certipay, please follow the steps below:
-
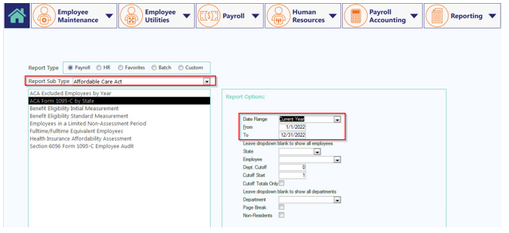
Click on the Reporting tab and where you see ‘Report Sub Type’, select ‘Affordable Care Act’.
-
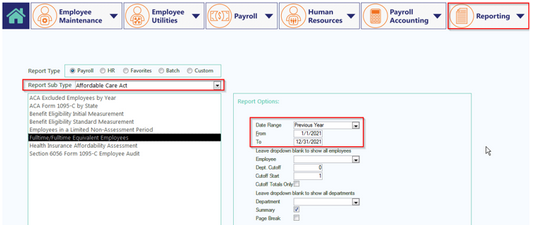
Under the Affordable Care Act Sub Type select the ‘Fulltime/Fulltime Equivalent Employees’ report
-
Update the Date Range to reflect ‘Previous Year’ and then click ‘Interactive View’. You also have the option to click ‘Summary’ to generate a summarized report
-
On this report, you will see all employees’ average hours worked per week and when you scroll all the way down, you will see the total average number of fulltime employees for the year. That number is what you can go by to determine whether you need to ACA report for the current year. If it’s under 50, then you are not required to ACA report, if it’s 50 or more, then you are required to report.
My Company is Required to report for ACA – Now What?
Now that you have determined your company is required to report for ACA, it is imperative that you go through the proper steps to ensure all medical benefits are setup correctly in Certipay. Elected as well as waived medical benefits will also need to be attached to employee profiles to ensure ACA compliance. Please review the ACA Compliance Medical Benefit set Up guide located in the Benefits section that offers step by step instructions on how to update Certipay. You may also want to refer to the ‘How to use the ACA Section 6056 Form 1095-C Employee Audit report’ to certify you are auditing Certipay correctly. You can also call in or email Client Solutions for questions you may have as it relates to maintaining ACA compliance.
If you do not wish to do this on your own, Certipay offers two types of services for all your ACA compliance needs. If you would like to enroll in one of our services, please send an email to clientservices@certipay.com so that the Benefits team can review your control(s) and provide you with a quote.
ACA Services Offered By Certipay
-
ACA/Benefits Setup & 4th Quarter ACA Audit
$1750 base fee in addition to standard ACA filing fees (finalized quote will be provided once the Benefits team has reviewed your control(s) plan structure and company size). The following is included with this service:
-
Enter new plan year benefits that fall within the reporting year at the company level
-
Update employee payroll deductions/earnings
-
Attach employee benefit elections to HR profile
-
Overview of Offer of Coverage and Safe Harbor Codes
-
Profile update to report for non-benefit eligible employees in a Limited Non-Assessment Period
-
Personalized training to maintain compliance for New Hires and Terminated employees
-
Assist with completion of the ACA Electronic Transmittal (required to have Certipay report on your behalf)
-
4th quarter audit of ACA data prior to generating and submitting ACA forms to the IRS
-
4th Quarter ACA Audit
$700 base fee in addition to standard ACA filing fees (finalized quote will be provided once the Benefits team has reviewed your control(s) plan structure and company size). The following is included with this service:
-
Review medical benefits setup to verify all required fields are populated
-
Review Section 6056 Form 1095-C Employee Audit report to determine any employees that need to be addressed for accurate reporting
-
Advised the client on any updates that are needed and how to update the company level/employee profile properly
Note: The above 4th quarter ACA audit does not include data entry. The benefits specialist will notify the client on any items that need to be reviewed and updated.
**Please also Note: If you use I-Enroller or any Benefit Interface, your benefits are already setup for you as a part of your renewal process, however ACA compliance is not guaranteed. If you choose to enroll in one of our ACA compliance services as an I-Enroller or Benefit Interface client, a discount will be applied for those ACA services.